A small medical centre in Rotorua may close due to carrying tens of thousands of dollars of unpaid patient fees – and two senior general practitioners say it won't be the last.
They say it reflects a wider issue that many other medical centres across the country could face if the government doesn’t step in now.
Meanwhile, a Te Whatu Ora Health New Zealand spokesperson has said she recognised that the funding model was not fit for purpose.
On Wednesday, Tiaho medical centre in Ōwhata, Rotorua, notified its patients that it was $33,000 in debt due to patients not paying for their doctors’ visits. The clinic changed its policies to remove all credit facilities with payment on the day of consultation.
In a letter it said: “This debt is unsustainable and requires urgent action to reduce it. If this is not achieved, there is a serious risk that the clinic will be unable to provide medical services to the community.
“This option is not the outcome the doctors and management want.”
On Thursday, several general practice bodies in New Zealand collectively rejected the government's proposed 5% increase in general practice funding, saying an increase of at least 14% is needed.
They were General Practice NZ, GenPro, Hauora Taiwhenua, the Royal NZ College of General Practitioners, the Practice Managers Association and the College of Primary Care Nursing.
They've given Te Whatu Ora a counterproposal including workforce solutions and a request for extra funding.
Royal NZ College of General Practitioners president Samantha Murton said most medical centres probably carry a reasonable amount of debt, but she didn't believe $33,000 was reasonable.
Struggling clinic not alone
“Tiaho is not alone, and I think lots of practices are struggling with how we make ends meet.”
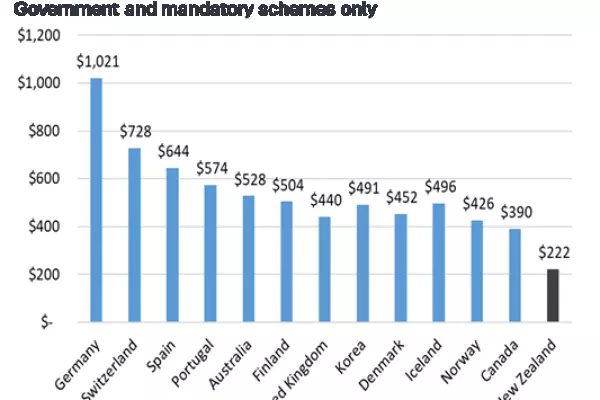
Murton said the portion of the money that goes into the community compared with the whole health budget is really small – about $1.039 billion out of a $26b budget.
“Proportionately, we get somewhere around 4-5% of the total health budget when we provide 90% of care in New Zealand.
“However, a 5% shift in their budget would make a 100% shift in ours.”
Murton said there was a government review of the funding 'capitation' formula and how it would work to match health needs. With capitation funding, practices are paid a fixed sum for each patient enrolled, no matter how many services they provide.
The government came up with a 9% deficit that primary care was missing out on, she said.
“Although they've got the evidence, they haven't put the money in yet.”
Murton said across all practices throughout the country, there's been a 6% increase in patient visits.
“If that 6% didn't come to us, they'd be going to the hospitals, and the hospitals would never recover.
“We see somewhere around, you know, 80,000 patients a day.
“So, even if we said, 'Okay, we're not going to see 2,000 of them' – that's 2,000 people that will go to hospitals.
“So, the tiniest proportion of movement for us in our sector makes a massive change in the hospital sector.”
Murton said the government had set up a working group to investigate the capitation model, but primary care needed to be prioritised urgently.
“We have these engagements and we talk these things through and then it feels like it doesn't land.
“How long do you leave something until it becomes a disaster?"
She said that was the problem – that everyone just continues to wait.
“We watched workforce numbers go down, we watched burnout increase, we watched nursing salaries reduce dramatically and people leaving for overseas. But the combination of all those things is going to come home to roost unless we do something right now.”
Closure a red flag
Bryan Betty, chair of General Practitioners NZ, said the Tiaho clinic being faced with closure due to financial strains was a red flag and showed that there is significant pressure on the health system.
“These types of issues arising are really, really concerning and that needs to be addressed by Te Whatu Ora and the government.
“We've seen a lot of stress right throughout the country.
“There's a real issue in New Zealand with the funding model and the way we fund general practice. And this is a really, really distressing situation to start to arise.”
Betty is based at Porirua Union and Community Health Service in Cannons Creek as GP and clinical director. His clinic provides services to more than 7,000 patients, mainly Māori, former refugees and Pasifika, 90% of them high-needs, a similar demographic to Tiaho.
He said there are thousands of practices around the country, all managed differently.
“It demonstrates a problem with carrying debt and that’s occurring in lots of different places.
“Financially, there needs to be more money put into primary care. It has not been dealt with for a number of years now. And we're starting to see these problems emerge in the system.”
Betty said there was an urgent need to focus on primary care and how general practice community medical care is supported.
“Basically, the majority of medical care in this country is provided by primary care practice.
“And it's part of the health system that needs to be backed and financially viable, going forward, especially in those areas of high need, where there are equity health issues."
More complex health conditions
He said it was really important to understand that clinics are seeing patients with increasingly complex health conditions, which leads to bigger workloads for health professionals.
“In high-needs areas, we get a very high concentration of complex patients. And that puts additional pressure and stress on the practices.”
Betty said primary care providers are seeing a lot of financial stress within the communities they support.
“We see a lot of patients who can't afford the co-payments. Although practices like ours have capped co-pay at $19, that does produce stress on the practice."
He said it limited the number of staff a practice could take on.
"And obviously, in the worst-case scenarios, that may start to compromise the financial viability of that practice, which, again, for communities is incredibly difficult.”
Betty said Tiaho’s situation is quite extreme, but it’s a real concern that closures are starting to happen because they have flow-on effects.
“One is additional stress and pressure, obviously, on other medical centres when the system is working at capacity.
“And number two, you’ll see additional pressure put on hospitals, especially emergency departments.
“And thirdly, for the patients themselves and their finances.
“It's a very stressful situation if that were to happen.”
Model is not fit for purpose
Emma Prestidge, interim director of primary, community and rural national commissioning at Te Whatu Ora said the primary health care system is central to improving the health of all New Zealanders.
She recognised that the current capitation-based funding model is not fit for purpose.
“It is inequitable in that it does not account for ethnicity, health disparities, the concentration of complexity, or the burden of disease. This makes it difficult to direct investment to those in greatest need.”
The 5% uplift is the single largest increase to capitation supporting the 950 general practices across NZ in recent times, Prestridge said.
“This represents over $63.5 million in new and ongoing investment.”
Prestidge said additional investment lifted the total up to nearly 9%.
This included the initiatives Community Services Card, Very Low-Cost Access, and Zero Fees for under-14s. She said this will keep the patient co-payment levels at their existing rates.
“This is over $21.5m and represents over a third of the $63.5m of new investment and is to help support those general practices serving those people in our communities who have the lowest ability to pay.”
Te Whatu Ora has provided an annual uplift for two years running, she said.
“That is more than what the contractually agreed and independent calculations are that determine the cost pressure increase facing general practices.”
Prestidge said as well as the 5% uplift, Te Whatu Ora is investing further funding into general practice, including $102m for community care teams, $31m for the nursing workforce, $86m over four years for the equity capitation formula, $24m ongoing for equity capitation and $10.5m for immunisation services.