Pharmacists have welcomed health minister Andrew Little’s hint about expanding their role to include advice on minor ailments, and referral services. But general practitioners are not as keen.
In an interview for our newly launched investigative series ‘The Business of Health’, Little said he wanted pharmacists to do more.
“GPs have this thing that they should be doing everything; they don't need to be doing everything. There are other health professionals we can rely on to do stuff,” he said.
“There are things that pharmacists can do that you shouldn't need to have to go to a doctor for, like minor ailments and skin ailments.”
Pharmacy Guild chief executive Andrew Gaudin said expanding the role of community pharmacists could help keep New Zealanders out of hospital, with earlier and more convenient access to health services.
It would also remove avoidable workforce pressures on general practices and emergency departments in a cost-effective way, he said.
‘Pharmacists are not diagnosticians’
Christchurch GP and General Practice Owners Association (GenPro) deputy chair Dr Angus Chambers was not as thrilled with the comments.
“Pharmacists have great skills in medicine management, but they are not diagnosticians,” he said.
“There are many examples of misdiagnosis by pharmacists. Sometimes, skin conditions are a manifestation of a serious disease, so if you have not been trained in diagnosis, how would you know it is a minor ailment?”
Chambers agreed the whole primary care sector needed a funding boost, including pharmacists, whose skills could be used in a better way.
“It is unclear what the policy is here. Do they want to reduce the number of GPs to replace them [with other health professionals], or do they want to support the GP workforce and supplement them?
“If [the minister] does not value GPs and wants to reduce their numbers because they are too expensive, he should just say so.
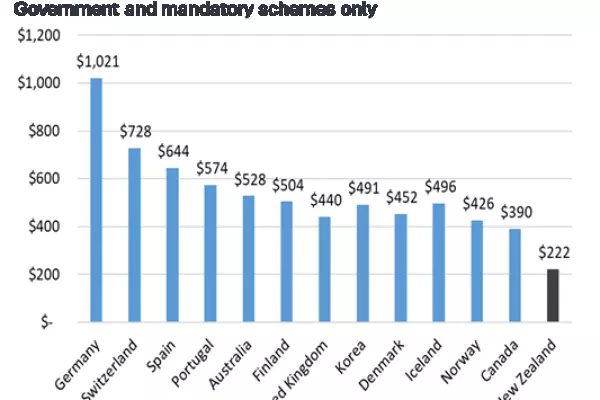
“We already have a very low number of GPs for our population compared to other countries.”
New Zealand has about 72 GPs per 100,000 people, while Australia has 116 GPs per 100,000, according to a 2021 College of General Practitioners report.
Filling the gaps
College of General Practitioners medical director Dr Bryan Betty said this country’s nationwide GP shortage was having a huge impact on hospital emergency departments as patients struggled to enrol with a practice or waited weeks for appointments.
GPs have been warning the government of the worsening shortage for at least a decade, Betty said.
They've pleaded for more funding to make general practice a more attractive prospect for medical school graduates.
Using pharmacists to fill the gaps was not a good solution, he said.
There was already increased collaboration between GPs and nurse practitioners, health improvement practitioners, pharmacists and other health professionals.
Collaboration was important but it couldn't solve underfunding and the workforce shortage, he said.
International research suggests that countries with higher GP densities have lower mortality rates.
A United States study found that 10 extra GPs per 100,000 people reduces the probability of cancer, respiratory and cardiovascular deaths by around 1%.