General practitioners have hit back at comments from health minister Andrew Little on the $490 million covid-19 funding they received last year, calling them “inappropriate” and “disingenuous”.
Tensions are rising between Little and GPs as Te Whatu Ora is due to share the results of a major review into the primary care funding model.
BusinessDesk asked Little if he was confident primary care was funded enough, as part of a series on the business of health.
He pointed to extra funding GPs received for the pandemic response: “Did they talk about the $490 million extra that went into primary care in the last year alone, just for care in the community? Because I find very few primary care entities talk about that."
GP practices received money for every patient testing positive for covid-19 so they could provide whatever support was needed, he said.
“When I got covid, I got two text messages the whole time – from the time I notified to the time I was deemed over it. Two text messages. The funding we provided was way more than the cost of two text messages."
“For some practices, for the vulnerable patients they made phone calls, which is the right thing to do. And in some cases, they sent a practice nurse around to very vulnerable patients to check things were OK.
“But, actually, a lot of money went to GP practices during that time and significantly increased their revenue.”
Having your cake
Christchurch GP and General Practice Owners Association (GenPro) deputy chair Angus Chambers said one-off funding could not solve years of underfunding.
“You can't have your cake and eat it, too.
"You might argue it would be a waste of health resources to spend a lot of time on presumably healthy individuals like Andrew Little. Now he is whining about not getting more contact when it would be taking care away from people who need it more, so it's pretty inappropriate what he said here.”
Practically overnight, general practices faced huge costs to protect patients and staff and provide testing, vaccination and care for covid-positive patients – on top of their usual workload, Chambers said. GPs racked up overtime, locum costs and premium rates for extra staff to compete with district health boards setting up parallel testing and vaccination clinics.
“Some GPs were working seven days a week, late at night, checking on people."
The covid funding was “pretty generous” and “propped general practices up” but it was not enough to solve long-standing issues, Chambers said.
“Why do they begrudge having paid [the extra covid funding] and expect it to pay for everything until the end of time? It’s basic financial illiteracy.
“Andrew Little has never had to run a business. I don’t think he understands that if GP practices ran with a deficit the way DHBs have run over so many years, they would all be out of business or in court.”
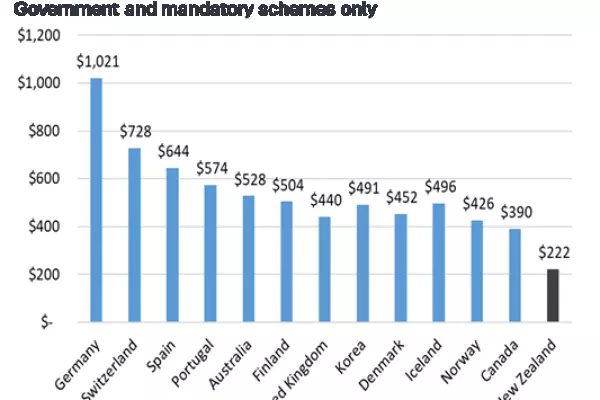
Hospitals got a 13.9% increase in funding in this year’s budget and primary care got 4.1%, according to the Federation of Primary Health, which described the discrepancy as a “gaping hole”.
“The government is investing billions of dollars into the restructure of management tiers and additional bureaucracy whilst imposing real-terms funding cuts on front-line [primary care] services,” the federation said in a statement earlier this year.
"Patients will increasingly be unable to access essential services unless the gross historic underfunding is addressed."
College of General Practitioners medical director Dr Bryan Betty said the level of care Little received from his GP had been defined by the Ministry of Health itself.
The covid funding did not change the fact that “primary care is underfunded in this country”, he said.
The funding model
GPs have two main sources of funding. The government provides 'capitation' funding, paid for each patient enrolled with a practice. GPs also charge fees to patients, which are effectively capped by the government.
GPs receive extra funding for running public health vaccination and screening campaigns. In the past three years, they received extra funding for the pandemic response.
GenPro chief executive Philip Grant said the government controlled all sources of funding for GPs, who had no right of negotiation over it. The government had kept GP funding below inflation over several years, while hospitals increasingly transferred more care into the community.
Chambers said the underfunding, combined with a GP shortage, had led to the worst wait times for primary care he had ever seen, and many people were struggling to enrol with a practice.
This, in turn, meant emergency departments around the country were under overwhelming pressure, he said.
Primary care nurses went on strike at the end of October, asking the government to increase capitation funding so GPs could pay them the same rate as hospital nurses, who earn up to 20% more.
A letter from Little, published on GenPro’s website, said a Te Whatu Ora review of capitation funding was due to be completed in June this year.
BusinessDesk asked Te Whatu Ora to provide more information about the review. The request was turned into an Official Information Act request, which takes up to 20 working days to be processed.
Grant said the sector was waiting to hear the results of the review.
“There is increasing urgency to address the sustainability of essential frontline general practices. For another review to be delayed and no action to be taken is disappointing,” he said.
“It feels a bit disingenuous [for the minister] to now be questioning the funding that went into GPs that were at the frontline of the covid response overnight, protecting NZ as requested by the minister and the ministry."