Very high-need general practices would need a funding increase of up to 231% to function properly, a review has found.
The government commissioned the Sapere Research Group earlier this year to review how general practitioners (GPs) are funded, as part of the health reforms.
The review was completed in July but kept under wraps until it was proactively released on Nov 16.
GPs, who are desperate for a funding increase, have voiced frustration at the delay. But Te Whatu Ora board chair Rob Campbell told BusinessDesk at a post-board meeting media briefing last week that the review’s findings were not a priority.
Te Whatu Ora had not commissioned the review, he said, and “producing a conclusion” on primary care funding was still months away.
Funding inadequate
GPs have two main sources of funding. The government provides 'capitation' funding, paid for each patient enrolled with a practice. The funding takes into account age and sex but does not account for ethnicity or deprivation.
GPs also charge fees to patients, which are effectively capped by the government.
The Health Transition Unit within the department of Prime Minister and Cabinet commissioned Sapere to review the capitation formula this year.
“The goal was to address a number of fundamental problems with the existing formula, and particularly to find an approach that responds to health needs appropriately,” the report said.
The report found that general practice revenue “lies below the likely true cost of delivering care at current levels”, and modelled the funding increases needed.
Capitation funding should be based on age, sex, ethnicity, deprivation and morbidity, the report said.
For very high-need practices, this would lead to an increase in capitation funding between 34% to 231%, “depending upon the level of benchmarking chosen”.
The modelling was based on the resources needed to “deliver higher than historic levels of care to priority populations, to represent a new normal”.
For most practices, the median modelled increase was between 10% and 20% of current capitation revenue, the report said.
“The current approach systematically underfunds services for Māori, by not recognising patterns of higher need and historical underutilisation by Māori. It embeds historical inequity".
Primary care funding “does not align with patient need”, the report said.
“This means that services that have a higher than average proportion of people with high health needs are not funded adequately to deliver care to their patients.
"This is a serious deficiency in a core part of New Zealand’s health system.”
GPs operating at a loss
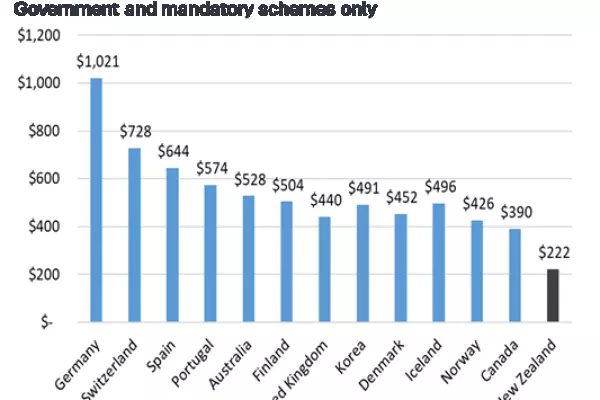
Capitation funding in 2021 was $1.114 billion – about $231 per enrolled patient.
Sapere calculated GP practice's current net deficit at $137m per annum (spread across all GP practices), at current levels of funding and costs.
“This implies that general practice makes a 7.6% loss each year. We are not in a position to confirm whether or not this profit margin would be typical for general practice, though we suggest that, given the sentiment that general practice is underfunded, our result of an average 7.6% loss seems realistic,” the report said.
“The situation is considerably worse for practices with a high-need population.”
Funding was only one aspect of what was needed to make primary care viable in Aotearoa, the report warned.
An increase in the number of GPs and support staff would be needed to improve equity of access to care.
“The viability of primary care services in the future depends critically upon the supply of the primary care workforce, and the distribution of services both geographically and demographically."
The review being made public comes as GP owners' association GenPro is campaigning to ‘Save Your Family Doctor’.
GenPro chair Tim Malloy said Kiwis are waiting longer to see their GP, and practices are struggling to stay afloat due to workforce issues, increased workloads and underfunding.
This was putting avoidable pressure on the rest of the health system and directly impacting the health of patients, he said.